Click to Get 2 FREE Boxes/Cans
Click to Get 2 FREE Boxes/Cans
Only New Customers! Click HERE to Get 2 Extra Boxes/Cans for Free With Your First Order.
Only New Customers! Click HERE to Get 2 Extra Boxes/Cans for Free With Your First Order.
BABY FORMULA
Offering new parents top-quality European infant formula from renowned brands like HiPP, Holle, Kendamil, and more. If you’re uncertain about which product to choose, our Formula Finder can help you make the best decision for your baby.
Baby Food
Offering new parents a premium selection of European baby foods, including jars, pouches, cereals, and snacks from esteemed brands like HiPP and Holle.
Do You Have to Warm Up Formula?
by Agustina Fernandez June 06, 2023 6 min read

When formula feeding, you're going to prepare hundreds of bottles throughout your baby's first months of life, so knowing how to do it safely and efficiently can save you lots of time and mental energy!
On busier days or during life on the go, warming up your baby's formula might not be realistic. If you find yourself in a pickle, you may be wondering, is feeding your baby cold formula safe?
This blog will put an end to the cold vs. warm formula debate as we walk you through the benefits and drawbacks of feeding your little one bottles at various temperatures.
Table of contents
Do You Have to Warm Up Formula?
To avoid beating around the bush, the simple answer to this question is no, baby formula does not have to be warmed up. Serving your baby formula that is room temperature or cold is safe as long as all general guidelines for storing and preparing the formula are followed.
That being said, parents often do choose to warm infant formula simply because many babies prefer warm bottles. If this is the case with your baby, all you have to do is place your baby's bottle in a bowl filled with warm water, run the bottle under a stream of warm tap water, or use a handy-dandy baby bottle warmer.
While babies may have a preference for this warmer temperature, if you are consistently giving them a cold bottle, they will likely get used to it as many babies drink cold formula happily!
What’s the best temperature to serve infant formula at?
Ultimately, it is safe to feed your baby cold, room temperature, or warm bottles. As long as it is not too hot (no more than 98.6℉ or 37℃), the best temperature will be based on your baby's preference. The reason babies may prefer formula that is warmed or at room temperature is that it's closer to the temperature of warm breast milk. 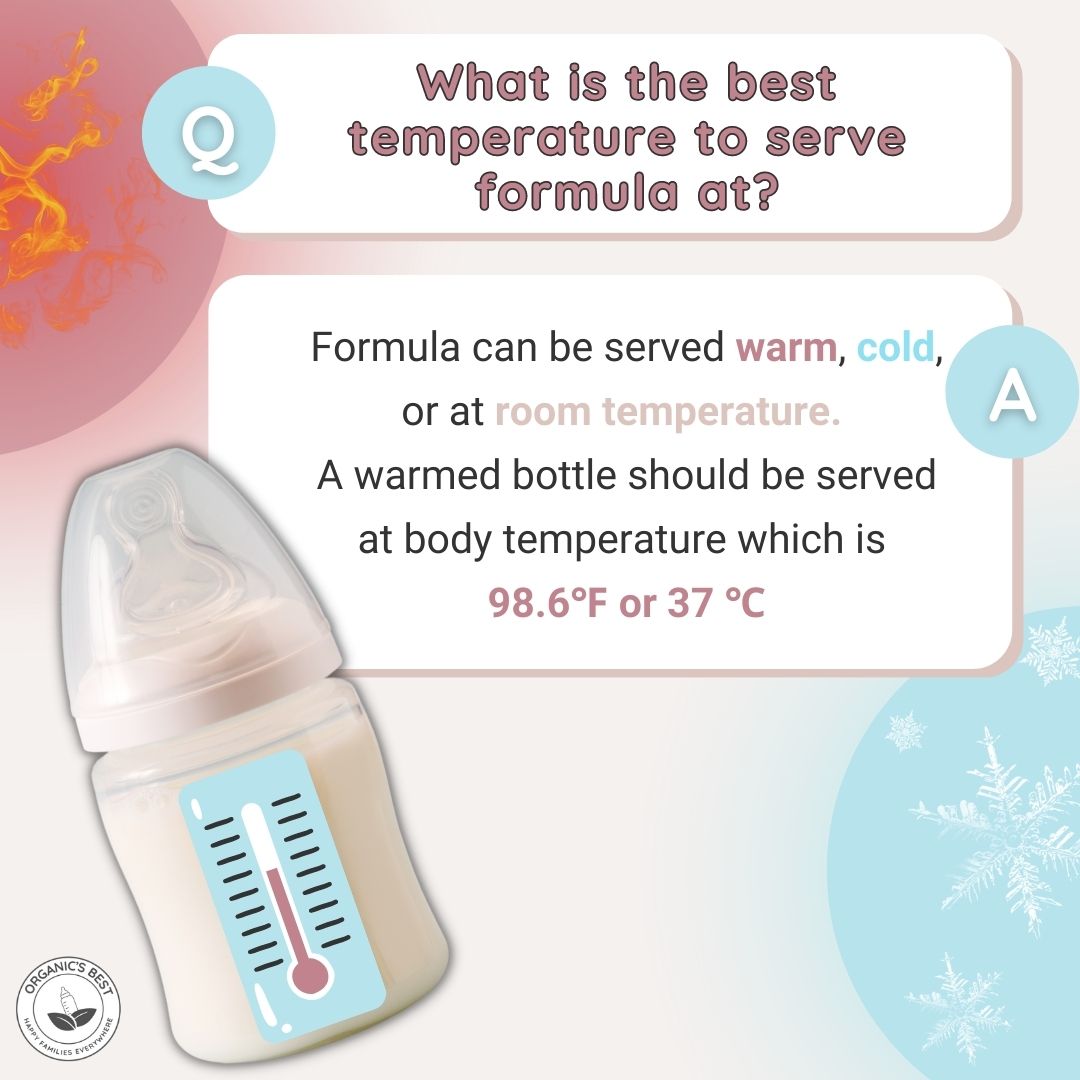
If you do choose to warm your child's formula, there are a few guidelines we recommend following:
-
A warmed bottle should be served at body temperature which is 98.6℉ or 37℃.
-
After boiling water, waiting it to cool to 70°C (158°F), and mixing it with formula powder, test the temperature of the bottle by dabbing a couple of drops on your wrist; it should feel lukewarm.
Does Warm Formula Have Any Benefits?
Technically speaking, there can be risks associated with warming formula compared to a formula served cold, simply due to the potential of overheating if you do not check the temperature.
As long as you safely prepare the warm formula, there are some benefits:

-
Some babies are picky about temperature and warmed formula can encourage them to drink their bottle, which ensures that they get enough calories and nutrients.
-
Premature babies may also benefit from having their formula warmed as certain studies show it can improve formula tolerance.
Is warm formula easier for babies to digest?
When it comes to premature infants, this might be the case, as a study showed that infants who were fed breast milk between 32 and 34 degrees Celsius had fewer gastric residuals (remaining fluids in the stomach after a feeding) than infants who were fed breast milk between 22 and 24 degrees Celsius.
However, this finding is specific to babies born prematurely. There is no evidence to indicate that the temperature of formula makes it easier or harder to digest in full-term infants. Although, some parents anecdotally find that warming formula does reduce their babies' tummy troubles.
Does warm formula cause less gas?
First and foremost, it is normal for infants to experience gas from time to time. This is most often caused by swallowing air during bottle feedings, from crying, or due to sucking their pacifier.
While some parents report anecdotally that warmer formula seems to reduce gassiness, there is limited scientific evidence to confirm that the temperature of the formula affects gas production in infants.
When preparing formula, it's important to use water that has been boiled and then cooled to a minimum of 70°C (158°F) to ensure it's free of contaminants. Once mixed, the formula should be further cooled to a comfortable feeding temperature if necessary, especially if you plan to serve it cold.
If you do use cold water, it can be harder for powdered formula to dissolve (even if you vigorously shake the bottle) and this can form more bubbles and foam, and thus, more gas. This is why it's important to always follow the manufacturer's instructions for formula preparation and storage.
Learn More: Gassy Baby: How to Help Relieve Your Baby's Gas
Does warm milk help babies sleep better?
While there is no scientific evidence to suggest that warm formula helps babies sleep better, anecdotally some parents find that incorporating warm formula as part of their baby's bedtime routine may help the child relax and prepare for rest.
The Pros and Cons of Feeding Your Baby Cold Formula

Pros 👍
-
Quicker preparation
-
Convenient for traveling
Cons 👎
-
It may take some time for your baby to not mind cold formula if they aren't used to it
-
If a baby is not feeding well, it might be hard to feed your baby cold formula
-
Unwarmed formula may be harder for premature babies to tolerate
How Do You Cool a Bottle of Formula? ❄️
Follow these steps to prepare cold formula:
-
Cool the bottle down by putting it in an ice bath or under cold running tap water
-
Keep the prepared formula in the fridge
-
Storing formula in the freezer is not recommended because it can cause the formula to separate and degrade some of its nutritional content.
How Do You Warm Up Baby Formula? 🔥
Follow these steps to prepare warm formula:
-
Warm the bottle by putting it in a bowl of warm water, under running warm water, or in a bottle warmer (more on how to use this safely in the next section).
-
Test the water before serving to make sure it is lukewarm-not hot.
-
Never use a microwave to heat formula, it may not heat things evenly and can lead to hot spots that could burn your baby's mouth.
Tips for Warming a Baby Bottle
We have already covered some guidelines, like testing the temperature of milk before serving, but there are a few more steps to consider when warming a baby bottle to keep it safe for your baby.

-
Do not use a microwave to heat baby bottles, as this can create hot spots, which can potentially burn your baby's mouth, throat, and esophagus.
-
If you are using a bottle warmer, make sure to do so with caution as it can be challenging to get the right temperature. It's best to begin by sticking to the lower heat settings and adjusting accordingly.
-
Choose a bottle made using high-quality material that is BPA-free.
Risks of Heating Formula
When formula gets too hot many of the beneficial properties can disappear and if heated incorrectly, either using a microwave or bottle warmer, your baby can get injured. This is why you must check the temperature of their formula before serving it and take precautions to avoid overheating your baby's formula.
Can You Reheat Formula?
Prepared powdered infant formula should be served and used within 2 hours of preparation and within 1 hour from when feeding begins. If your baby does not finish their bottle after an hour, you'll have to discard any of the remaining formula. This means that formula cannot be reheated, because used formula can harbor bacteria from your baby's mouth.
Learn More: How Long is Formula Good For?
Conclusion
Preparing your baby's bottle is just one of the many steps on the never-ending to-do list of a new parent, so it helps to know that you don't have to fret about the temperature. Feeding your baby cold or warmed formula is perfectly fine in most circumstances and it all comes down to the preference of your little one. So long as you follow the safe feeding guidelines as outlined in this article, then making up baby bottles will be a breeze!
Disclaimer:
Please be aware that this information is based on general trends in babies, and it is not medical advice. Your doctor should be your first source of information and advice when considering any changes to your child’s formula and when choosing your child’s formula. Always consult your pediatrician before making any decisions about your child’s diet or if you notice any changes in your child. Breastfeeding is the best nutrition for your baby because breast milk provides your child with all the essential nutrients they need for growth and development. Please consult your pediatrician if your child requires supplemental feeding. |
Agustina Fernandez
Dr. Agustina Fernandez earned her medical degree from the prestigious Universidad Nacional de Córdoba, Argentina. With a deep-rooted passion for pediatrics, Dr. Fernandez is currently on the path to specializing in children's healthcare. Recently, she has delved into the vital field of infant nutrition. Her research interests include breastfeeding, infant formula, and baby food in little ones’ formative years. Dr. Fernandez's commitment to this area of study underscores her dedication to ensuring the health and well-being of children from their earliest days.
Leave a comment
Comments will be approved before showing up.
Also in Organic Infant Nutrition and Health Blog

10 Winter Activities for Kids and Toddlers
by Agustina Fernandez January 06, 2026 8 min read
Read More
How to Choose The Best Infant Formula: A Guide to EU Organic Formulas
by Agustina Fernandez January 05, 2026 14 min read
Read More
Best Formula for Breastfed Babies 2026 Guide
by Agustina Fernandez January 05, 2026 15 min read
Read More
Reviewed by Dr. Po-Chang Hsu, MD, MS
-

Dr. Po-Chang Hsu: Medical Reviewer of Organic's Best Blog
Dr. Hsu received his medical degree from Tufts University in Boston, Massachusetts, and holds a Master’s of Science degree from both Harvard University and Tufts University.
